U-M Team Receives NIH Grant for Collaborative Research to Speed ARDS Diagnosis
University of Michigan researchers examine if molecular compounds in exhaled breath could lead to improved diagnosis and tracking of acute respiratory distress syndrome (ARDS).
Contacts
Michele Santillan
Communications Manager,
Biomedical Engineering
mssantil@umich.edu
Kate Murphy
Marketing Communications Specialist,
U-M Max Harry Weil Institute
mukately@med.umich.edu
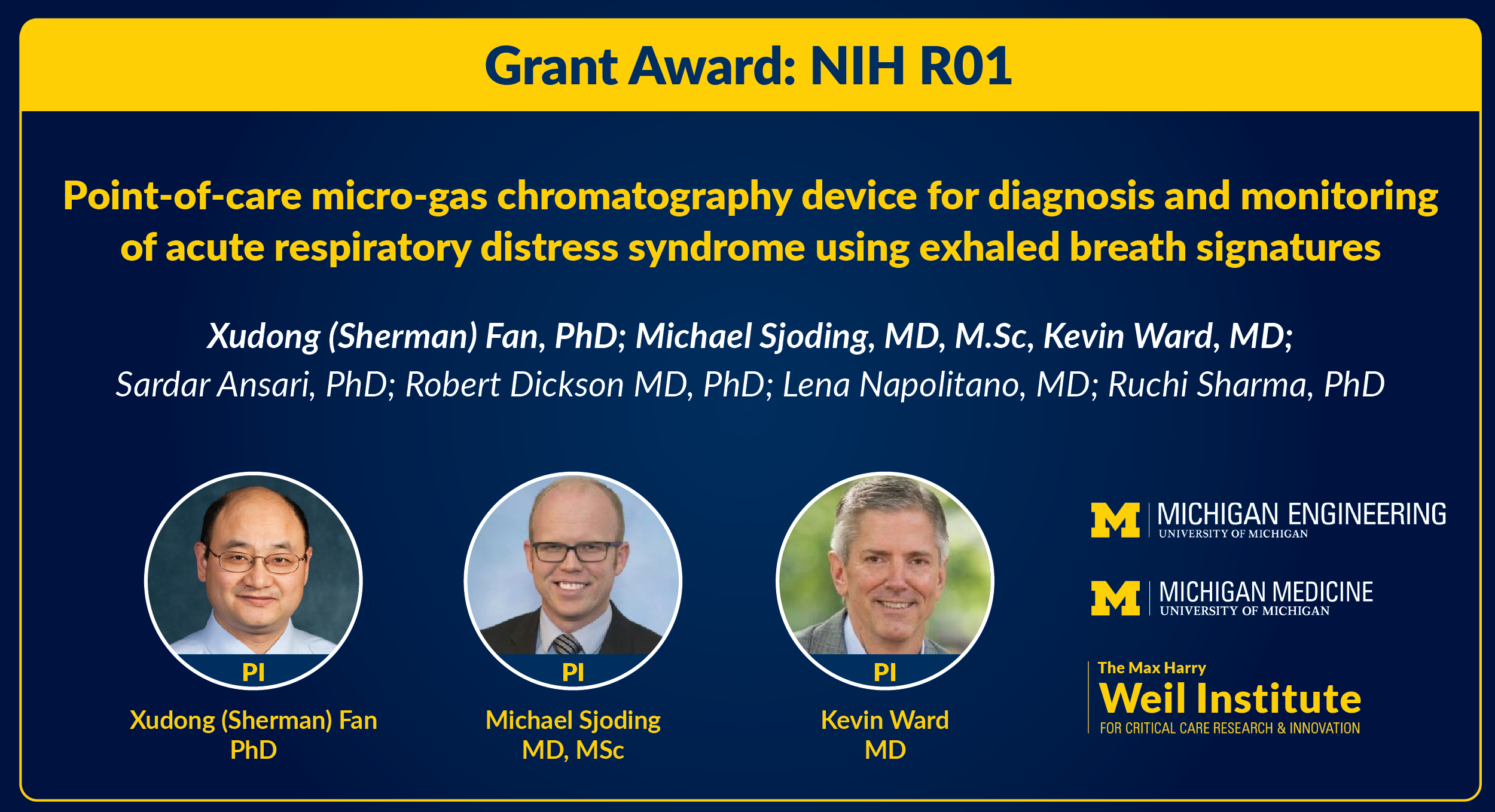
ANN ARBOR, MI – Through a $4.17M National Health Institutes (NIH) grant, a University of Michigan team of biomedical engineers, medical clinicians and data scientists from the Max Harry Weil Institute for Critical Care Research and Innovation is collaboratively researching ways to develop a portable, non-invasive breathalyzer-type device and corresponding algorithm to quickly and accurately diagnose acute respiratory distress syndrome (ARDS), and subsequently track its progress.
This research—led by co-investigators Xudong (Sherman) Fan, Ph.D., Richard A. Auhll Endowed Professor of Engineering, Professor, Biomedical Engineering, Associate Director of the Weil Institute; Michael Sjoding, M.D., Associate Professor, Division of Pulmonary and Critical Care Medicine, Internal Medicine, Associate Director of the Weil Institute; and Kevin Ward, M.D., Professor of Emergency Medicine and Biomedical Engineering, Executive Director of the Weil Institute—seeks to detect ARDS more quickly and more accurately than is currently possible and will help determine if patients’ health is recovering or declining. The researchers’ project is expected to improve clinical decision-making and enable the introduction of earlier treatment, with an ultimate goal of improving outcomes for those suffering from ARDS.
ARDS is a life-threatening lung injury that allows fluid to leak into the lungs and makes breathing difficult, killing 74,000 people each year in the United States. “ARDS is an important condition in the ICU because it has a high mortality rate and requires specific management approaches,” added Dr. Sjoding. “The problem is that sometimes it can be difficult to recognize, so we are desperate for new tools for ARDS detection and monitoring.”
Unfortunately, ARDS is common, costly, and responsible for long-term morbidity. For example, according to Dr. Fan, the average cost of an intensive-care-unit (ICU) patient requiring mechanical ventilation is $5,000 – $10,000 per day, with an incremental cost of $1,500 per day for mechanical ventilation. This monetary figure does not account for the human costs involved, such as mortality risks for ARDS patients and the emotional and financial toll of illness on patients, families, and caregivers.
Unfortunately, the understanding of patient susceptibility and the underlying pathobiology of ARDS is currently incomplete. Clinical diagnosis is based on the Berlin ARDS clinical criteria, which is imprecise in application, and there currently are no established biomarkers to support ARDS diagnosis.
Patients with ARDS are frequently missed in time by clinicians and frequently do not receive evidence-based treatments to improve patient outcomes. Additionally, only crude clinical markers, such as oxygenation, are currently available to track ARDS progression and resolution, making it difficult to identify patients likely requiring advanced therapies with enough time to evaluate the effectiveness of their response. There is a significant unmet clinical need for early, rapid, and accurate ARDS diagnosis, as well as clinical trajectory monitoring of ARDS to ensure resolution with treatment.
The U-M interdisciplinary team will leverage their expertise in biomedical engineering, data science, pulmonary diseases, and critical care by using exhaled volatile organic and inorganic compounds (VOCs and VICs) to more accurately identify ARDS among patients with acute hypoxemic respiratory failure. U-M researchers have used similar processes of VOC/VIC analysis to detect COPD, asthma, and COVID-19 in patients. Their work on ARDS will also require the development of new machine learning and artificial intelligence (AI) approaches to analyze the high-density data provided by the device.
The U-M team will focus on the patients’ VOCs and VICs, many of which are related to inflammatory and metabolic processes in the lungs and other organs. Such VOCs/VICs could be used as biomarkers for ARDS if they could be measured simultaneously and precisely in real time. Gas chromatography (GC) is the gold standard for analyzing complex vapor mixtures like breath, but current technologies to make these measurements are difficult to bring to the bedside due to their large size.
By using the innovative point-of-care gas analyzer developed and tested in this proposal, the team is expected to gain fundamental insights into the presence and dynamics of VOCs/VICs in exhaled breath which present as inflammatory and metabolic markers of ARDS pathophysiology. Most importantly, the portable GC technology will bring molecular diagnostics to the bedside, enabling earlier initiation of ARDS treatments that improve outcomes, as well as novel trajectory monitoring to inform prognosis and downstream critical-care decision-making.
Specifically, this proposal will build upon the team’s preliminary GC technology–a prototype portable micro-GC device–which they developed and used to measure exhaled VOCs and discover patterns distinguishing ARDS from other causes of acute hypoxic respiratory failure in a small group of adult patients.
"ARDS is an important condition in the ICU because it has a high mortality rate and requires specific management approaches. The problem is that sometimes it can be difficult to recognize, so we are desperate for new tools for ARDS detection and monitoring."
Michael Sjoding, MD
Associate Professor, Pulmonary and Critical Care Medicine; Associate Director, Weil Institute
Michigan Medicine
“Our device is actually portable and weighs about 6 or 7 pounds, at most,” explained Dr. Fan. “And it can be used to continuously monitor ARDS patients' breath through our ventilation machines over multiple days.”
To advance the device for clinical use, the researchers must now validate preliminary findings and obtain robust time-series data to identify the breath biomarker signatures that enable disease detection and trajectory monitoring. They will also evaluate the added benefit of measuring VICs within the system on top of the VOCs measurement, which they expect will improve device performance because many VICs (e.g., nitric oxide) provide important additional markers of inflammation.
The team is launching the process of recruiting 400 patients to participate in their research. Dr. Fan noted that patients will be followed by examining how the initial diagnosis is made, as well as their progression and response to therapeutic treatments over time.
“This grant will really accelerate our work towards establishing exhaled breath as a viable diagnostic tool for earlier identification of ARDS and monitoring patients with Acute Respiratory Distress Syndrome until its resolution,” concluded Dr. Sjoding.
“This is another great example of the Weil Institute’s utilization of convergence science taking deep expertise from the fields of biomedical engineering, data science, physiology, and multiple medical disciplines to create and test a technology that could potentially transform not only the care of patients with ARDS, but eventually other life-threatening inflammatory diseases such as sepsis.” said Dr. Ward. “The NIH grant recognizes the value of our approach, and it is envisioned that the award will propel us to eventual regulatory approval of the technology.”
Other members of the team include Robert Dickson, M.D., Associate Professor, Pulmonary and Critical Care Medicine, Microbiology and Immunology, Deputy Director of the Weil Institute; Lena Napolitano, M.D., Professor and Associate Chair, Surgery, Associate Director of the Weil Institute; Sardar Ansari, Ph.D., Research Assistant Professor, Emergency Medicine, Director of the Weil Institute Data Science Team; and Ruchi Sharma, Ph.D., Research Investigator, Biomedical Engineering, Member of the Weil Institute.
Conflict of Interest Disclosures
Dr. Xudong Fan is a co-inventor of the technologies that may be used in this project. These technologies have been licensed to third-party companies, Nanova, ChromX Health, and RUA Diagnostics Inc., in which Dr. Fan has financial interest.
Dr. Kevin R. Ward is a co-inventor of the technologies that may be used in this project. Dr. Ward has a financial interest in RUA Diagnostics.
Dr. Sardar Ansari is a co-inventor of technologies that may be used in this project.
Dr. Ruchi Sharma is a co-inventor of technologies that may be used in this project.
The University of Michigan has a financial interest in Nanova Environmental, Inc., ChromX Health Co. Ltd., and RUA Diagnostics Inc.
About the Weil Institute (formerly MCIRCC)
The team at the Max Harry Weil Institute for Critical Care Research and Innovation (formerly the Michigan Center for Integrative Research in Critical Care) is dedicated to pushing the leading edge of research to develop new technologies and novel therapies for the most critically ill and injured patients. Through a unique formula of innovation, integration and entrepreneurship that was first imagined by Weil, their multi-disciplinary teams of health providers, basic scientists, engineers, data scientists, commercialization coaches, donors and industry partners are taking a boundless approach to re-imagining every aspect of critical care medicine. For more information, visit weilinstitute.med.umich.edu.